Lyme Disease and Pregnancy

The multi-faceted, complex issue of Lyme disease and pregnancy, maternal-fetal transmission of the Lyme disease causing spirochete Borrelia burgdorferi, and congenital Lyme (a baby infected with the bacteria that causes Lyme disease at birth) is one of great importance to those who have been impacted and to medical providers who provide support and care to their patients.
We trust that providing you with this fact-based information will open and bridge new conversations on this issue. We will be updating this page with new information, research opportunities and resources as it becomes available.
The Lyme disease spirochete, Borrelia burgdorferi, can be transmitted from a pregnant mother, across the placenta, to her baby in the womb. This has been historically reported by the US Centers for Disease Control (CDC), National Institutes of Health (NIH), World Health Organization (WHO) and Canadian Federal Health Authorities.
The US CDC and Health Canada currently acknowledge the risk of maternal-fetal transmission of Lyme disease on their respective websites.
In a July 4, 1989 article (1) in the New York Times titled Medical Science Steps Up its Assault on Lyme Disease, Dr. David Axelrod, the New York State Health Commissioner at the time was interviewed and quoted. When asked about Lyme and pregnancy, he stated this:
"We do know that the Lyme bacterium crosses the placenta. Most babies born of mothers with treated Lyme disease have been healthy, yet the long-term impact of this disease on the developing fetus and newborn is not entirely clear."
We trust that providing you with this fact-based information will open and bridge new conversations on this issue. We will be updating this page with new information, research opportunities and resources as it becomes available.
The Lyme disease spirochete, Borrelia burgdorferi, can be transmitted from a pregnant mother, across the placenta, to her baby in the womb. This has been historically reported by the US Centers for Disease Control (CDC), National Institutes of Health (NIH), World Health Organization (WHO) and Canadian Federal Health Authorities.
The US CDC and Health Canada currently acknowledge the risk of maternal-fetal transmission of Lyme disease on their respective websites.
In a July 4, 1989 article (1) in the New York Times titled Medical Science Steps Up its Assault on Lyme Disease, Dr. David Axelrod, the New York State Health Commissioner at the time was interviewed and quoted. When asked about Lyme and pregnancy, he stated this:
"We do know that the Lyme bacterium crosses the placenta. Most babies born of mothers with treated Lyme disease have been healthy, yet the long-term impact of this disease on the developing fetus and newborn is not entirely clear."
Dr. Axelrod’s quote from over 30 years ago rings true today. We do know that the Lyme disease causing spirochete can cross the placenta and infect a fetus/baby, this has been acknowledged by many experts in the field. Significant knowledge gaps remain regarding how Lyme disease impacts pregnancy and furthermore, very little information exists on the potential for long-term health impacts of babies born to mothers with gestational Lyme. Ultimately, collaborative, multi-sectoral research on this issue will open new doors for better diagnostics, treatment, healthcare professional education and resources, and support for families and children impacted
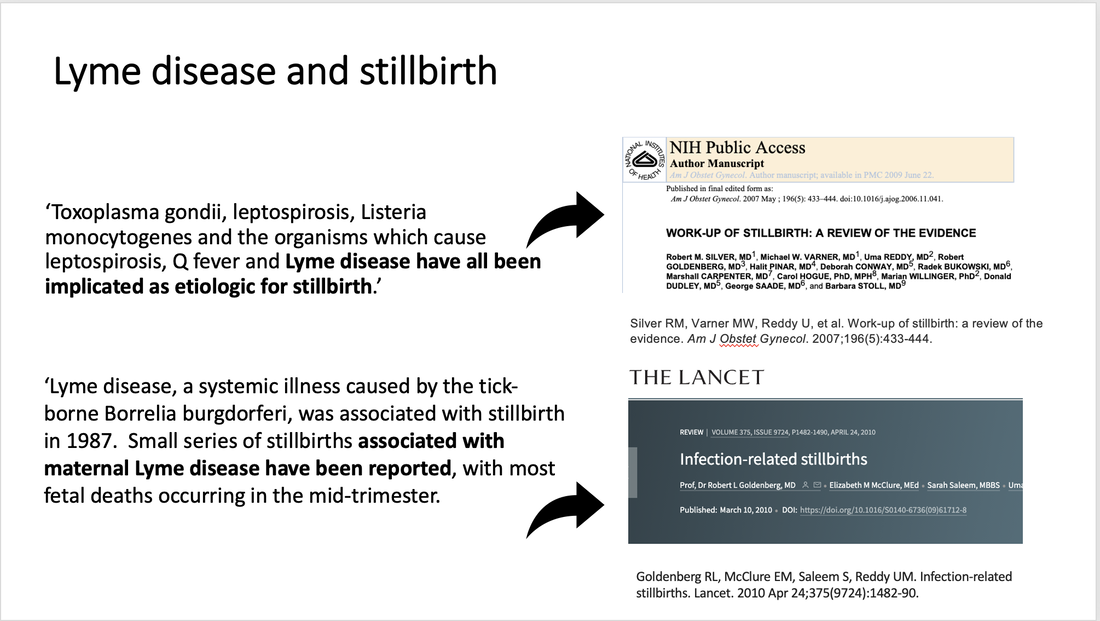
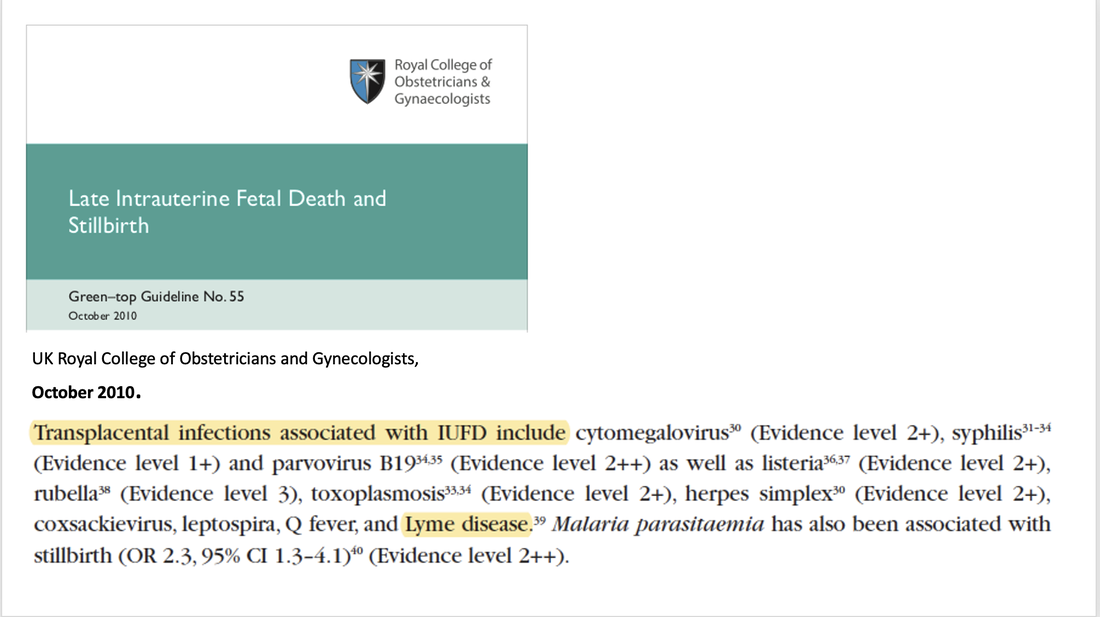
A 1991 committee opinion (3) by The American College of Obstetricians and Gynecologists (ACOG) acknowledges spirochetes can cross the placenta with resultant stillbirth. The UK Royal Society of Obstetricians and Gynecologists (4) has listed Lyme disease as one of the infectious organisms which can cross the placenta leading to late intrauterine fetal death and stillbirth. Expert reviews (5-9) on stillbirth in the American Journal of Obstetrics and Gynecology, Obstetrical and Gynecological Survey, Seminars in Fetal and Neonatal Medicine, and the Lancet have identified Borrelia burgdorferi as being either associated with, or etiologic for stillbirth.
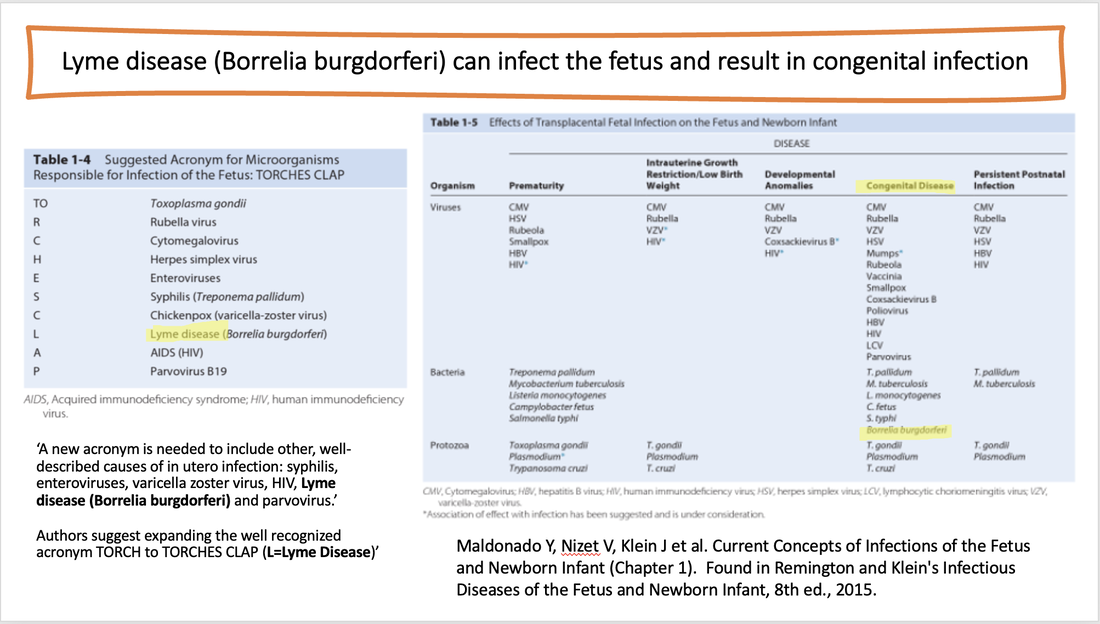
The current (8th) edition of Remington and Klein Infectious Diseases of the Fetus and Newborn Infant, a reference medical textbook, lists Lyme disease as one of the microorganisms known to cross the placenta, resulting in congenital infection. (10)
A paper published on the histopathology of Lyme borreliosis (10) states, ‘Uterine involvement in stage II Lyme borreliosis is a significant factor in pregnancy since it may result in transplacental transmission of B. burgdorferi to the fetus. One of us has recently encountered cases of decidual necrosis with inflammation in patients with intrauterine infection due to B. burgdorferi (de Koning, unpublished data).’
Overview of Cases:
Cases of miscarriage, stillbirth, neonatal death and babies/children with congenital Lyme infection have been reported including cases whereby the pregnant mother was bitten by a tick and didn’t receive medical treatment, cases of pregnant women with late-stage Lyme, and cases of subclinical or asymptomatic infection (where the pregnant mother had no recall of a tick-bite or erythema migrans rash in pregnancy).
Healthy Babies and Pregnancy Outcomes:
There have also been many cases reported with good pregnancy outcomes and healthy infants born to mothers with treated Lyme disease.
Adverse Outcomes in Pregnancy
A wide range of fetal or neonatal adverse outcomes have been documented with Lyme and Pregnancy. In many cases it wasn’t proven that these outcomes were directly caused by the Lyme bacteria. More research is needed to see if there is a definitive link between some of these adverse pregnancy outcomes and gestational Lyme infection.
Some of the adverse outcomes reported include:
Clinical manifestations reported in the newborn include:
Treatment in Pregnancy: Prompt diagnosis and treatment of Lyme disease in pregnancy is associated with good pregnancy outcomes. There have been a few cases whereby Lyme bacteria was identified in placenta or in fetal tissue, or other adverse outcomes were noted despite antibiotic treatment in the mother. Currently there are differing medical opinions regarding the length and type treatment for Lyme in pregnancy ranging from oral antibiotics to IV antibiotics. (Citations 74-82)
A meta-analysis performed in a recent systematic review by Waddell et al identified treated Lyme in pregnancy is associated with fewer adverse outcomes (11%, 95%CI 7–16) versus untreated (50%, 95%CI 30–70). A study by Lakos et al reviewed data from 95 women with Lyme borreliosis during pregnancy over a 22 year span. Adverse outcomes were identified in 12.1% of parentally treated women, 31.6% of orally treated women and 60% of untreated women, thus drawing attention to a significantly higher rate of adverse pregnancy outcomes in untreated cases.
Treatment Guidelines for Lyme and Pregnancy and Congenital Lyme Infection:
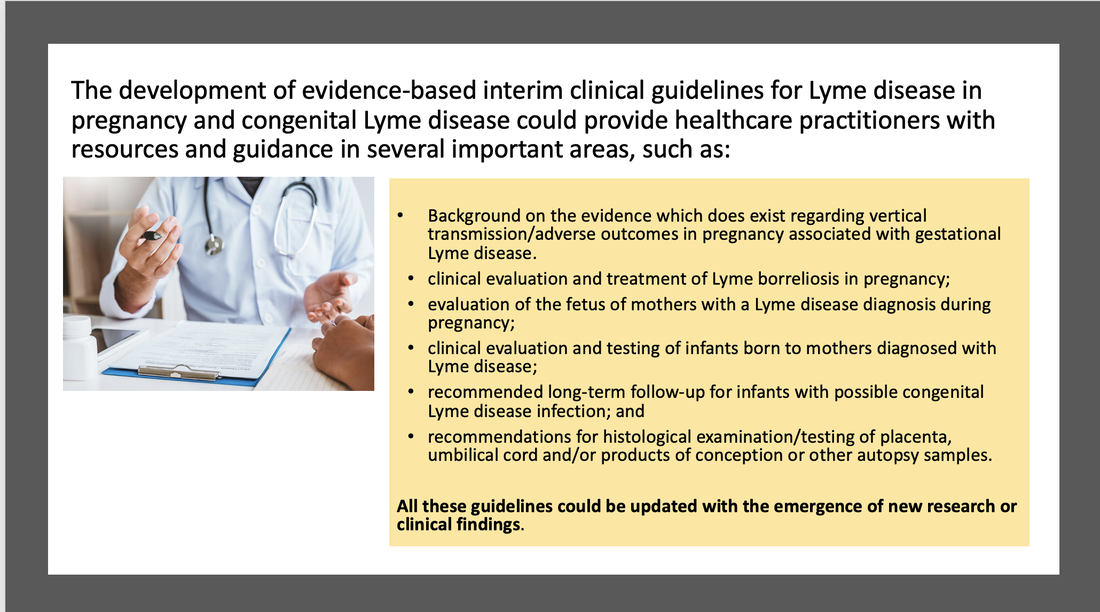
Many health care professionals (including primary-care practitioners and OB-GYNs) may not be aware that this alternate mode of transmission is even possible. Pregnant women with Lyme (or those desiring to become pregnant) may have to advocate for assessment, treatment and monitoring of themselves and their baby after birth.
Standardized clinical guidelines providing recommendations for diagnosis, treatment and follow-up of Lyme borreliosis for both mother and exposed fetus/infant have never been created. Other zoonotic infectious diseases such as Zika, Chagas disease and West Nile Virus do have these guidelines.
Interim guidelines could be developed based on evidence available to date and be updated as new research findings are reported. Without clear guidance, practitioners/clinicians may be uncertain of how to manage cases of gestational and congenital Lyme disease, which may lead to misdiagnosis or inadequate management.
A standardized assessment tool to guide clinical evaluation, treatment/management and follow-up of infants born to mothers with Lyme during pregnancy could include:
Overview of Cases:
Cases of miscarriage, stillbirth, neonatal death and babies/children with congenital Lyme infection have been reported including cases whereby the pregnant mother was bitten by a tick and didn’t receive medical treatment, cases of pregnant women with late-stage Lyme, and cases of subclinical or asymptomatic infection (where the pregnant mother had no recall of a tick-bite or erythema migrans rash in pregnancy).
Healthy Babies and Pregnancy Outcomes:
There have also been many cases reported with good pregnancy outcomes and healthy infants born to mothers with treated Lyme disease.
Adverse Outcomes in Pregnancy
A wide range of fetal or neonatal adverse outcomes have been documented with Lyme and Pregnancy. In many cases it wasn’t proven that these outcomes were directly caused by the Lyme bacteria. More research is needed to see if there is a definitive link between some of these adverse pregnancy outcomes and gestational Lyme infection.
Some of the adverse outcomes reported include:
- spontaneous miscarriage and stillbirth
- premature delivery
- early neonatal death
- intrauterine growth restriction
Clinical manifestations reported in the newborn include:
- respiratory distress and neonatal sepsis
- low birth weight and hyperbilirubinemia (jaundice)
- hypotonia (poor muscle tone)
- neurologic abnormalities including hydrocephalus, neurologic dysfunction and developmental delay
- dental anomalies including hypoplastic enamel
- cardiac malformation and myocardial dysfunction
- genitourinary (urinary tract) abnormalities
- ocular (eye) manifestations including cortical blindness
- dermatological (skin) manifestations including cavernous hemangioma, newborn rash
- orthopedic (bone) abnormalities including clubfoot, joint contractures, syndactyly, and transverse metaphyseal bands seen on x-ray.
Treatment in Pregnancy: Prompt diagnosis and treatment of Lyme disease in pregnancy is associated with good pregnancy outcomes. There have been a few cases whereby Lyme bacteria was identified in placenta or in fetal tissue, or other adverse outcomes were noted despite antibiotic treatment in the mother. Currently there are differing medical opinions regarding the length and type treatment for Lyme in pregnancy ranging from oral antibiotics to IV antibiotics. (Citations 74-82)
A meta-analysis performed in a recent systematic review by Waddell et al identified treated Lyme in pregnancy is associated with fewer adverse outcomes (11%, 95%CI 7–16) versus untreated (50%, 95%CI 30–70). A study by Lakos et al reviewed data from 95 women with Lyme borreliosis during pregnancy over a 22 year span. Adverse outcomes were identified in 12.1% of parentally treated women, 31.6% of orally treated women and 60% of untreated women, thus drawing attention to a significantly higher rate of adverse pregnancy outcomes in untreated cases.
Treatment Guidelines for Lyme and Pregnancy and Congenital Lyme Infection:
Many health care professionals (including primary-care practitioners and OB-GYNs) may not be aware that this alternate mode of transmission is even possible. Pregnant women with Lyme (or those desiring to become pregnant) may have to advocate for assessment, treatment and monitoring of themselves and their baby after birth.
Standardized clinical guidelines providing recommendations for diagnosis, treatment and follow-up of Lyme borreliosis for both mother and exposed fetus/infant have never been created. Other zoonotic infectious diseases such as Zika, Chagas disease and West Nile Virus do have these guidelines.
Interim guidelines could be developed based on evidence available to date and be updated as new research findings are reported. Without clear guidance, practitioners/clinicians may be uncertain of how to manage cases of gestational and congenital Lyme disease, which may lead to misdiagnosis or inadequate management.
A standardized assessment tool to guide clinical evaluation, treatment/management and follow-up of infants born to mothers with Lyme during pregnancy could include:
- Laboratory testing guidance
- Clinical Assessment Tools
- Treatment recommendations
- Recommendations for subspecialty consultation and support (cardiology, neurology, ophthalmology etc.)
- Recommendations for histological examination/ testing of placenta, umbilical cord tissue
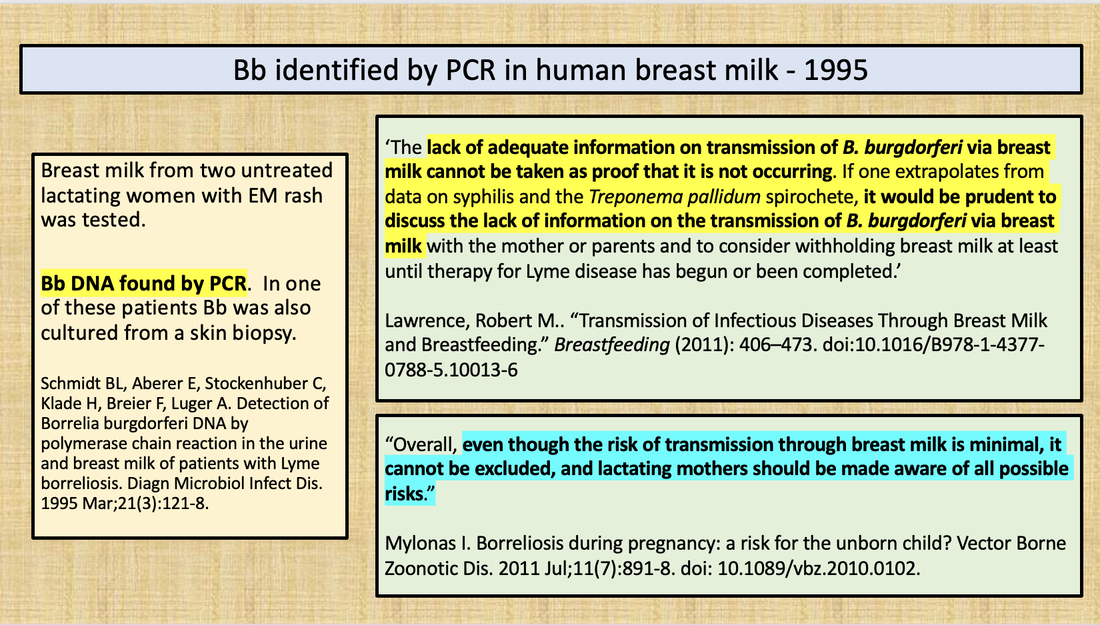
Breastfeeding: There is no direct evidence that nursing mothers infected with Lyme disease can transmit infection through their milk. Borrelia burgdorferi DNA has been identified by PCR in breastmilk from two lactating mothers. According to some experts, although transmission via breastmilk has not been reported, it cannot be excluded. Citations 83-85.
Prospective Studies Needed!
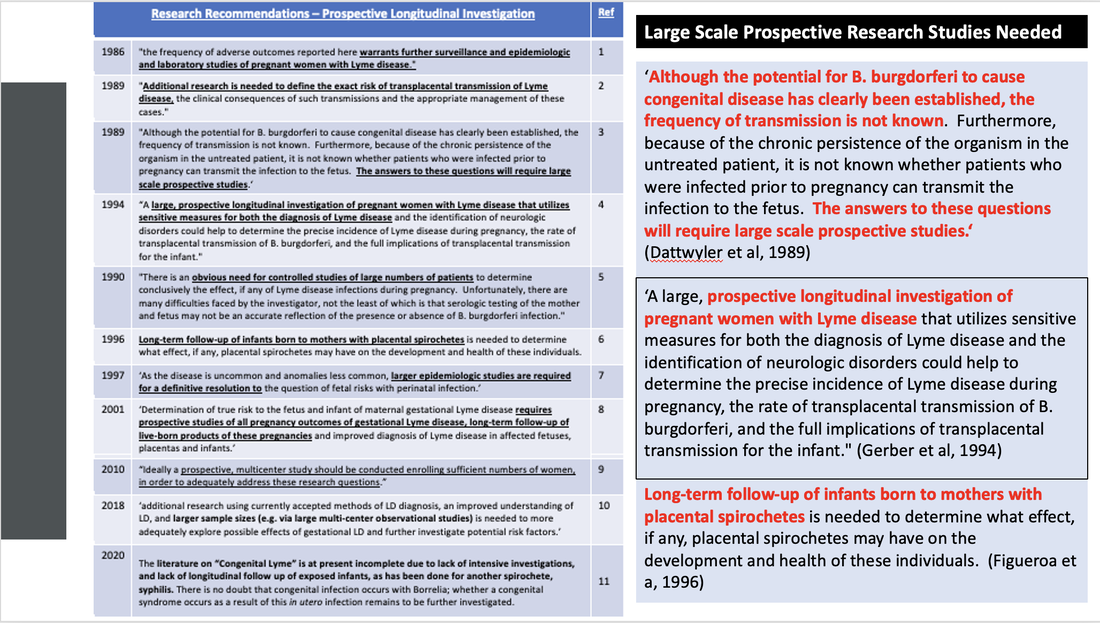
Mother to baby transmission of Lyme disease is vastly understudied. Many past researchers and investigators have highlighted the necessity and importance of large-scale prospective studies following mothers with Lyme and their babies over prolonged period as a critical next step.
According to one group of experts: "Although the potential for B. burgdorferi to cause congenital disease has clearly been established, the frequency of transmission is not known. Furthermore, because of the chronic persistence of the organism in the untreated patient, it is not known whether patients who were infected prior to pregnancy can transmit the infection to the fetus. The answers to these questions will require large scale prospective studies. Analysis of case reports and small studies offers us a perspective and some tentative guidelines for the diagnosis and treatment of this infection during pregnancy."
Mother to baby transmission of Lyme disease is vastly understudied. Many past researchers and investigators have highlighted the necessity and importance of large-scale prospective studies following mothers with Lyme and their babies over prolonged period as a critical next step.
According to one group of experts: "Although the potential for B. burgdorferi to cause congenital disease has clearly been established, the frequency of transmission is not known. Furthermore, because of the chronic persistence of the organism in the untreated patient, it is not known whether patients who were infected prior to pregnancy can transmit the infection to the fetus. The answers to these questions will require large scale prospective studies. Analysis of case reports and small studies offers us a perspective and some tentative guidelines for the diagnosis and treatment of this infection during pregnancy."
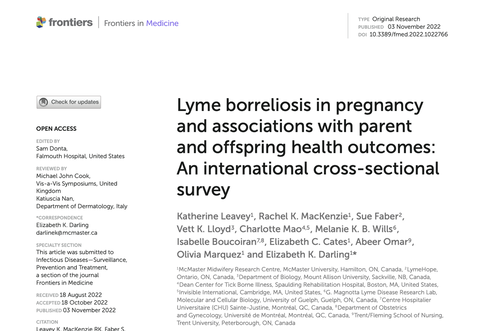
A pioneering research study: led by Dr. Liz Darling and team from McMaster University Midwifery Research Centre and collaborators titled Lyme borreliosis in pregnancy and associations with parent and offspring health outcomes: An international cross-sectional survey has been published and also calls for prospective studies.
From the paper: 'overall, this pioneering survey represents significant progress toward understanding the effects of LD on pregnancy and child health. A large prospective study of pregnant people with LD, combining consistent diagnostic testing, exhaustive assessment of fetal/newborn samples, and long-term offspring follow-up, is warranted.' A brief overview of this study can be found here:
From the paper: 'overall, this pioneering survey represents significant progress toward understanding the effects of LD on pregnancy and child health. A large prospective study of pregnant people with LD, combining consistent diagnostic testing, exhaustive assessment of fetal/newborn samples, and long-term offspring follow-up, is warranted.' A brief overview of this study can be found here:
Lyme Disease and Pregnancy: State of the Science & Opportunities for Research
An April 2021 webinar on Lyme and Pregnancy highlights important questions, research gaps and opportunities related to this subject matter. LymeHope has compiled a supplementary document to accompany our presentation for the webinar.
An April 2021 webinar on Lyme and Pregnancy highlights important questions, research gaps and opportunities related to this subject matter. LymeHope has compiled a supplementary document to accompany our presentation for the webinar.
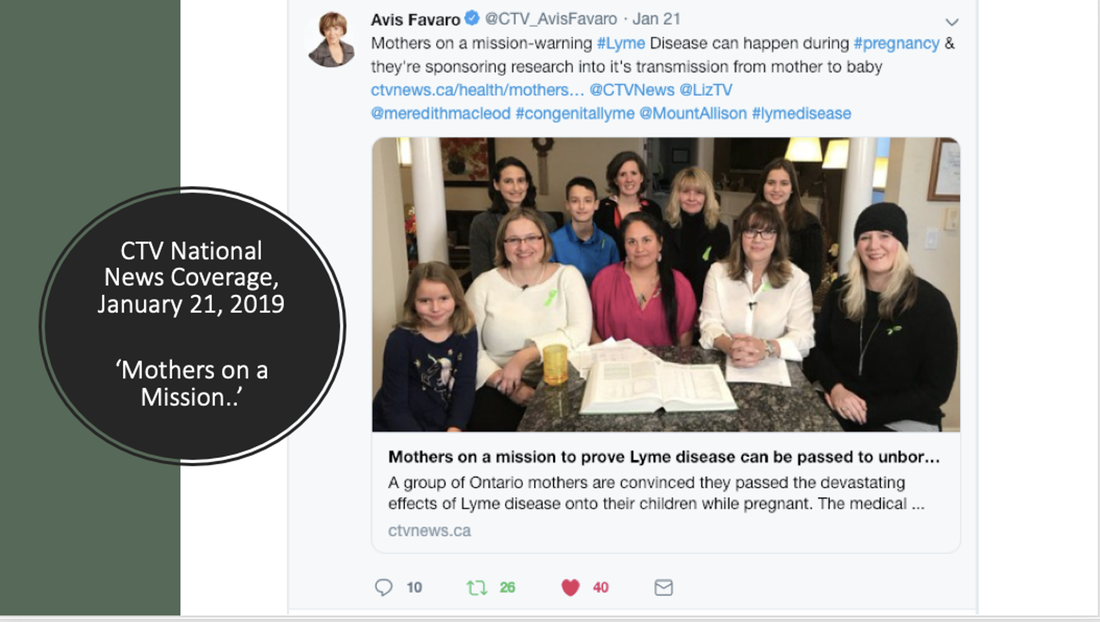
Patient Voice: A collective patient and advocacy voice, combined with opportunities within Academia and Government for research collaboration is making a difference.

Support for families: Mothers Against Lyme is an organization started by a group of mothers, and mother-advocates, concerned about the impact of Lyme Disease and its co-infections on pregnant women, children and families.
Their focus includes awareness, education, advocacy and community building, as they promote research that advances diagnosis, treatment and prevention. They have started a virtual 'meet-up' support group for parents who have children with Lyme disease in collaboration with Project Lyme. If you are interested in participating in the 'meet-up' or receiving newsletters, you can sign up on the Mothers Against Lyme website, through their 'Join Us' button.
Their focus includes awareness, education, advocacy and community building, as they promote research that advances diagnosis, treatment and prevention. They have started a virtual 'meet-up' support group for parents who have children with Lyme disease in collaboration with Project Lyme. If you are interested in participating in the 'meet-up' or receiving newsletters, you can sign up on the Mothers Against Lyme website, through their 'Join Us' button.
In Canada, CTV National News featured a national television news story on mothers concerned about congenital Lyme disease.
The LymeLight Foundation has compiled videos sharing stories of families impacted by congenital Lyme disease which can be accessed from their website. They also have resources specific to Lyme disease and Pregnancy.
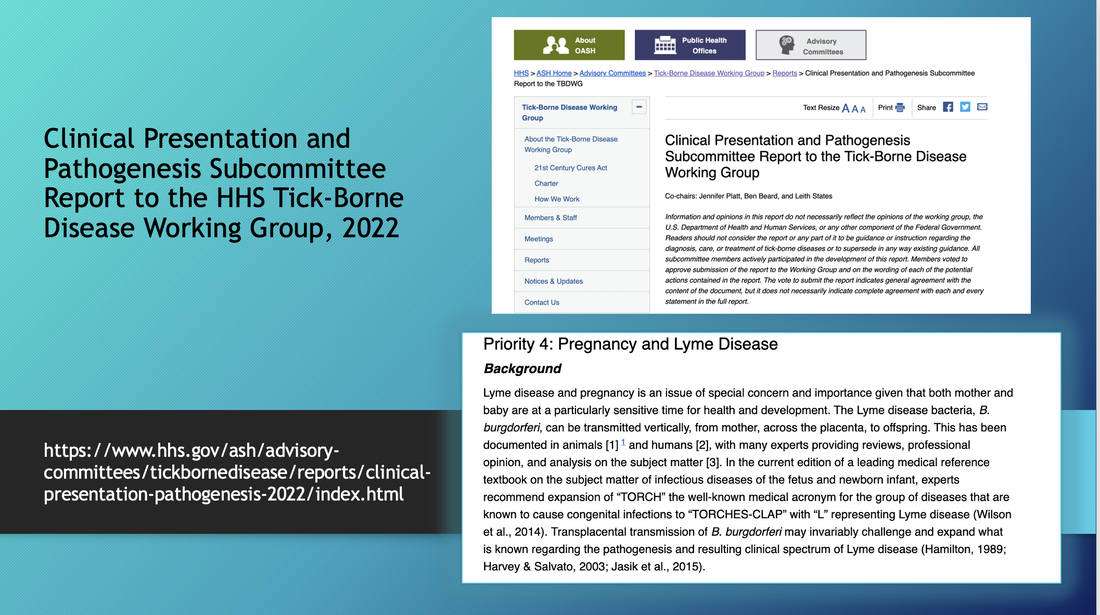
US Tickborne Disease Working Group:
A 202o US Tick-Borne Disease Working Group Report to Congress identified in Recommendation 8.3 ‘Further evaluation of non-tick bite transmission of Lyme disease, for example maternal-fetal transmission.’ The report also states, ‘Similarly, additional studies of potential congenital Lyme disease, and of persistent Lyme disease in undiagnosed and untreated infants resulting from maternal transmission of B. burgdorferi, could be helpful, as could patient registries.’
A 2022 Pathogenesis and Clinical Presentation subcommittee report to the Tick-borne Disease Working Group addressed Lyme and Pregnancy as one of several priorities (Priority 4) and provides an in-depth overview of the issue in their report including research gaps, opportunities and possible recommendations.
A 202o US Tick-Borne Disease Working Group Report to Congress identified in Recommendation 8.3 ‘Further evaluation of non-tick bite transmission of Lyme disease, for example maternal-fetal transmission.’ The report also states, ‘Similarly, additional studies of potential congenital Lyme disease, and of persistent Lyme disease in undiagnosed and untreated infants resulting from maternal transmission of B. burgdorferi, could be helpful, as could patient registries.’
A 2022 Pathogenesis and Clinical Presentation subcommittee report to the Tick-borne Disease Working Group addressed Lyme and Pregnancy as one of several priorities (Priority 4) and provides an in-depth overview of the issue in their report including research gaps, opportunities and possible recommendations.
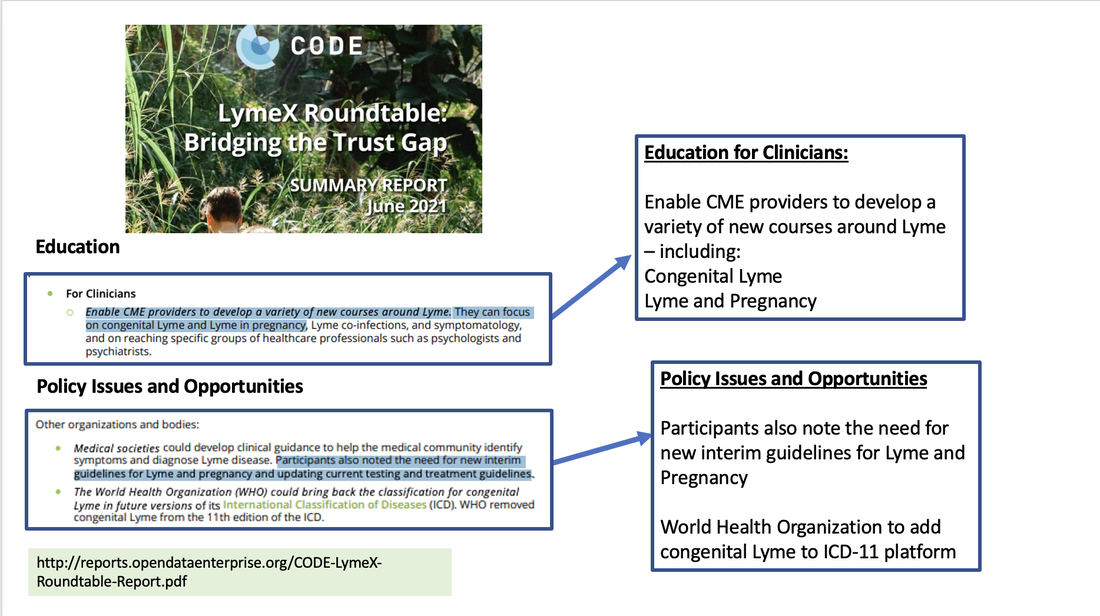
LymeX Roundtable Summary Report, 2021. In a recent summary report from a LymeX Roundtable, 'Bridging the Trust Gap' in the 'Policy Issues and Opportunities' section, participants identified the necessity for interim guidelines for Lyme and Pregnancy. In a section on 'Education' it was identified that CME courses could focus on gestational and congenital Lyme among other topics.
Banbury Meeting on Perinatal Transmission of Lyme disease. A 2022 Banbury Meeting (scientific think-tank) on Perinatal Transmission of of Lyme disease brought together scientists/researcher, clinicians, US Federal government representatives and leaders from Lyme disease organizations to examine the issue and identify new research opportunities.
Research and Knowledge Gaps:
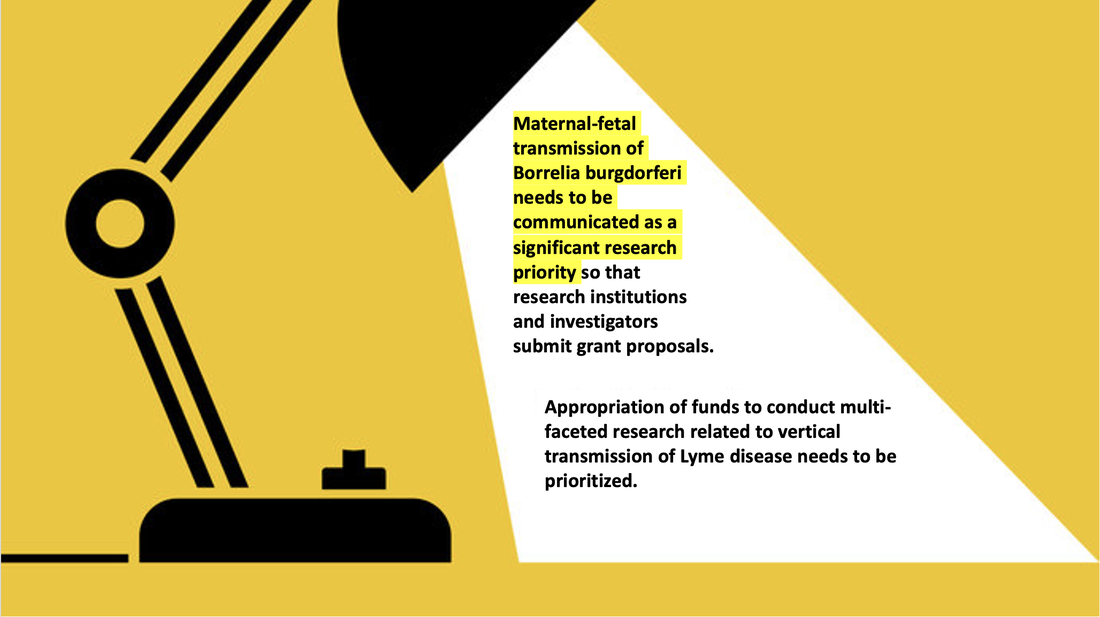
Significant knowledge gaps remain regarding how Lyme disease impacts pregnancy in cases of acute versus chronic or subclinical illness, including best diagnostic approaches to identifying infection in both mother and baby, best treatment approaches in a pregnant woman or in an infant who is symptomatic at birth.
Questions remain as how to identify a pregnant woman who may be infected but does not recall a tick-bite or EM rash, or the possibility of a latent or subclinical infection. Very little information exists on the potential for long-term health impacts of babies born to mothers with gestational Lyme. Clearly, the prevalence, incidence, clinical spectrum and potential long-term health consequences of infants exposed to Lyme in-utero must be further examined. Maternal-fetal transmission of Lyme disease need to be communicated as a significant research priority so that research institutions and investigators submit grant proposals. Appropriation of funds to conduct multi-faceted research related to vertical transmission of Lyme disease needs to be prioritized.
Significant knowledge gaps remain regarding how Lyme disease impacts pregnancy in cases of acute versus chronic or subclinical illness, including best diagnostic approaches to identifying infection in both mother and baby, best treatment approaches in a pregnant woman or in an infant who is symptomatic at birth.
Questions remain as how to identify a pregnant woman who may be infected but does not recall a tick-bite or EM rash, or the possibility of a latent or subclinical infection. Very little information exists on the potential for long-term health impacts of babies born to mothers with gestational Lyme. Clearly, the prevalence, incidence, clinical spectrum and potential long-term health consequences of infants exposed to Lyme in-utero must be further examined. Maternal-fetal transmission of Lyme disease need to be communicated as a significant research priority so that research institutions and investigators submit grant proposals. Appropriation of funds to conduct multi-faceted research related to vertical transmission of Lyme disease needs to be prioritized.
Next Steps:
Collaboration and innovation is required to investigate the complexities of Lyme and pregnancy, maternal-fetal transmission and congenital Lyme infection. State of the art science is required to investigate the research gaps and complexities of this alternate mode of transmission and will require a collaborative multi-disciplinary multi-stakeholder ‘relay-team’ approach, which values an integrative model of bringing together patients with lived experience, front-line clinicians, clinical researchers, and scientists to collectively identify, propose and carry out further investigation.
Collaboration and innovation is required to investigate the complexities of Lyme and pregnancy, maternal-fetal transmission and congenital Lyme infection. State of the art science is required to investigate the research gaps and complexities of this alternate mode of transmission and will require a collaborative multi-disciplinary multi-stakeholder ‘relay-team’ approach, which values an integrative model of bringing together patients with lived experience, front-line clinicians, clinical researchers, and scientists to collectively identify, propose and carry out further investigation.
References
- Altman, Lawrence K. Medical Science Steps Up its Assault on Lyme Disease. July 4, 1989. The New York Times. https://www.nytimes.com/1989/07/04/science/medical-science-steps-up-its-assault-on-lyme-disease.html
- Maldonado Y, Nizet V, O.Klein J, Remington J, Wilson C. Current concepts of Infections of the Fetus and Newborn Infant (Chapter 1). Found in Remington and Klein Infectious Diseases of the Fetus and Newborn Infant, 8th edition, 2015.
- ACOG Committee Opinion: Committee on Obstetrics: Maternal and Fetal Medicine. Lyme disease during pregnancy. Int J Gynecol Obset 1992, 39:59-60. https://pubmed.ncbi.nlm.nih.gov/1358705/
- Late Intrauterine Fetal Death and Stillbirth. Royal College of Obstetricians and Gynaecologists. Green-top Guideline No. 55, October 2010.
- Goldenberg, R. L., & Thompson, C. (2003). The infectious origins of stillbirth. American Journal of Obstetrics and Gynaecology, 189(3), 861– 873. doi:10.1067/s0002-9378(03)00470-8
- Silver RM, Varner MW, Reddy U, et al. Work-up of stillbirth: a review of the evidence. Am J Obstet Gynecol. 2007;196(5):433-444.
- McClure EM, Dudley DJ, Reddy UM, Goldenberg RL. Infectious causes of stillbirth: a clinical perspective. Clin Obstet Gynecol. 2010;53(3):635-645.
- McClure EM, Goldenberg RL. Infection and stillbirth. Semin Fetal Neonatal Med. 2009 Aug;14(4):182-9.
- Goldenberg RL, McClure EM, Saleem S, Reddy UM. Infection-related stillbirths. Lancet. 2010 Apr 24;375(9724):1482-90.
- Maldonado Y, Nizet V, Klein J et al. Current Concepts of Infections of the Fetus and Newborn Infant (Chapter 1). Found in Remington and Klein's Infectious Diseases of the Fetus and Newborn Infant, 8th ed., 2015.
- De Koning J., Duray PH. Histopathology of Human Lyme borreliosis. In: Weber K, Burgdorfer W (eds) Aspects of Lyme Borreliosis. Springer-Verlag Berlin Heidelberg 1993. ISBN-13:978-3-642-77616-
- Waddell LA, Greig J, Lindsay R, Hinckley AF, Ogden NH. A systematic review on the impact of gestational Lyme disease in humans on the fetus and newborn. PLoS ONE 13 (11): e0207067. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0207067
- Lakos, A., & Solymosi, N. (2010). Maternal Lyme borreliosis and pregnancy outcome. International Journal of Infectious Diseases, 14(6), e494e498. https://pubmed.ncbi.nlm.nih.gov/19926325/
- Schlesinger PA, Duray PH, Burke BA, Steere AC and Stillman MT. Maternal-Fetal transmission of the Lyme disease spirochete, Borrelia Burgdorferi. Ann Intern Med. 1985;103(1):67-8.
- MacDonald A. Gestational Lyme Borreliosis. Implications for the fetus. Rheum Dis Clin North Am. 1989 Nov;15(4):657-77
- Neubert, U. (1987): Erythema migrans in der Gravidität. Hautarzt; 38: 182-183.
- MacDonald AB. Human fetal borreliosis, toxemia of pregnancy and fetal death. Zentralbl Bakt Mikrobiol Hyg A. 1986 Dec;263(1-2):189-200.
- Maraspin V, Cimperman J, Lotric-Furlan, S et al. Erythema migrans in pregnancy. Wein Klin Wochenschr (1999) 111/22-23:933-940.
- MacDonald A, Benach J, Burgdorfer W. Stillbirth following Maternal Lyme Disease. New York State Journal of Medicine vol 87, Nov 1987.
- Lavoie PE, Lattner BP, Duray PH, Barbour AG, Johnson RC. Culture positive seronegative transplacental Lyme Borreliosis infant mortality (1987) Arthritis Rheum, 30(4), 3(suppl):S50
- Weber K, Bratzke H, Neubert UWE et al. Borrelia Burgdorferi in a newborn despite oral penicillin for Lyme borreliosis during pregnancy. Pediatric Infectious Disease Journal Vol 7, No 4, 286-289, 1988
- Horowitz R, Yunker LL. Lyme Disease and Pregnancy: Implications of Chronic Infection, PCR testing and Prenatal Treatment Case Presentation. 16th International Scientific Conference on Lyme Disease and other Tick-Borne Diseases. June 7, 8, 2003.
- Dattwyler R, Volkman D, Luft B. Immunologic aspects of Lyme borreliosis. Review of Infectious Diseases, Vol 11(6) 1989.
- Gasser R, Dusleag J, Reisinger E, et al. A Most Unusual Case of a Whole Family Suffering from Late Lyme Borreliosis for Over 20 Years. Angiology. 1994;45(1):85-86.
- Gardner T. Infectious Diseases of the Fetus and Newborn Infant. In: Remington JS, Klein JO, editors. Lyme Disease, Chapter 11. 5th ed. Philadelphia, PA: The W.B. Saunders Co.;2001. pp. 519-641.
- Lampert, R. Infantile multisystem inflammatory disease: another case of a new syndrome. Eur J Pediatr (1986) 144:593-596.
- Trevison G, Stinco G, Cinco M. Neonatal skin lesions due to a spirochetal infection: a case of congenital Lyme borreliosis? Journal of Dermatology, 36, 677, 1997.
- Lazebnik T, Zal'tsman P. A Case of Congenital Neuroborreliosis. St Petersburg Medical Academy of Postgraduate Education, St. Petersburg, Russia. 2005.
- Jones, CR., Smith H., Gibb E, Johnson L. Gestational Lyme Disease Case Studies of 102 Live Births. Lyme Times, Gestational Lyme Studies, Summer 2005, pp. 36-38.
- Onk, G., Acun C., Murat K., et al. Gestational Lyme disease as a cause of Congenital Hydrocephalus. J Turkish German Gynecol Assoc. Vol 6(2):156-157.
- MacDonald A. Gestational Lyme Borreliosis. Implications for the fetus. Rheum Dis Clin North Am. 1989 Nov;15(4):657-77
- Horst, H.: Borrelia burgdorferi-Infektionen in der Schwangerschaft. In: Hassler, D. (Hrsg): Infection Taschenbuch Lyme-Borreliose. MMV. Medizin Verlag, Munchen 1992, 85-91.
- Vanousova D, Nemcova A, Hulinska D, Schmiedbergerova R., Hercogova J. Transplacentární přenos borelií? Čes-slov Derm, 2007, roč. 82, č. 4, s. 218
- Spector, R., Rummelt, V., Folberg R. The Pathology of Congenital Lyme Borreliosis. Abstract 1466-27. Investigative Opthamology and Visual Science, Annual Meeting. May 2-May 7, 1993, Sarasota Florida. March 15, 1993. Vol 34, No 4.
- Burrascano J (1993) Failure of aggressive antibiotic therapy to protect the placenta from invasion by B. burgdorferi in a pregnant patient with Lyme borreliosis. 6th Annual International Science Conference on Lyme Disease and other Tick-borne Diseases. May 5-6, 1993, Atlantic City, NJ.
- Qureshi MZ, New D, Zulqarni NJ, Nachman S. Overdiagnosis and overtreatment of Lyme disease in children. Pediatr Infect Dis J. 2002 Jan;21(1):12-4.
- Hercogova J, Vanousova D. Syphilis and borreliosis during pregnancy. Dermatol Ther. 2008 May-Jun;21(3):205-9.
- Hulinksa, D., Votypka J., Horejsi J. Disseminated Lyme borreliosis and its laboratory diagnosis. Zpravy Epidemiologie A Mikrobiologie (SZU Praha) 2011:20(1)
- Patmas, M. Letter to the Editor. Persistence of Borrelia burgdorferi despite antibiotic treatment. Journal of Spirochetal and Tick-Borne Disease, Vol 1(4), 1994. Pp. 101.
- Figueroa R, Bracero LA, Aguero-Rosenfeld, M et al. Confirmation of Borrelia Burgdorferi spirochetes by polymerase chain reaction in placentas of women with reactive serology for Lyme antibodies. Gynecol Obstet Invest. 1996;41(4):240-3.
- Lakos, A., & Solymosi, N. (2010). Maternal Lyme borreliosis and pregnancy outcome. International Journal of Infectious Diseases, 14(6), e494–e498. doi:10.1016/j.ijid.2009.07.019 https://pubmed.ncbi.nlm.nih.gov/19926325/
- Maraspin V, Lusa L, Blejec T, Ružić-Sabljić E, Pohar Perme M, Strle F. Course and Outcome of Erythema Migrans in Pregnant Women. J Clin Med. 2020;9(8):2364.
- Silver HM. Lyme disease during pregnancy. Infect Dis Clin North Am. 1997. Mar;11(1):93-7.
- Alexander JM, Cox SM. Lyme disease and pregnancy. Infect Dis Obstet Gynecol. 1995;3(6):256-261.
- Schutzer SE, Jannigan CK, Schwartz RA. Lyme Disease During Pregnancy. CUTIS. Volume 47, April 1991. pp 267-268.
- Williams CL., Strobino BA. Lyme disease transmission during pregnancy. Contemporary Ob/Gyn, June 1990. Pg. 48-54.
- Luft BJ, Dattwyler RJ. Lyme Borreliosis. Current Clinical Topics Infectious Disease. 1989; 10:56-81.
- Edly S. Lyme Disease During Pregnancy. New Jersey Medicine. Vol 87 (7), July 1990.
- Dennis, D. Epidemiology. Chapter 4. In: Coyle PK. (ed) Lyme disease. Mosby Year Book, 1992. ISBN: 1-55664-365-9
- Cartter M, Hadler J, Gerber M, Mofenson L. Lyme Disease and Pregnancy. Connecticut Medicine. Volume 53 (6), June 1989.
- Adams FG. Connecticut Epidemiologist. Epidemiology Section. State of Connecticut Department of Health Services. Pregnancy and Lyme Disease. March 1989, Vol 9(2).
- CDC Prevention Guidelines Database (Archive). Vector-Borne Diseases (Lyme disease, Japanese Encephalitis, Yellow Fever.). Publication date 08/01/1991.
- Pinger, R. R., Hamm, R. H., & Sinsko, M. J. (1989). Lyme disease: a review and an outlook for Indiana. Indiana medicine : the journal of the Indiana State Medical Association, 82(4), 268–272.
- Schell, W., Davis JP. Lyme Disease: A Clinician’s Guide. State of Wisconsin, Department of Health and Social Services. Division of Health. Bureau of Community Health and Prevention. Section of Acute and Communicable Disease Epidemiology. January, 1989.
- O'Brien JM, Martens MG. Lyme disease in pregnancy: a New Jersey medical advisory. MD Advis. 2014 Winter;7(1):24-7. PMID: 25375870.
- Dotters-Katz, Sarah K. MD*; Kuller, Jeffrey MD†; Heine, R. Phillips MD‡ Arthropod-Borne Bacterial Diseases in Pregnancy, Obstetrical & Gynecological Survey: September 2013 - Volume 68 - Issue 9 - p 635-649.
- Shapiro E, Gerber M. Borrelia Infections: Lyme Disease and Relapsing Fever. Chapter 17. Found in Remington and Klein's Infectious Diseases of the Fetus and Newborn Infant, 7th ed., 2011.
- Elliott DJ, Eppes SC, Klein JD. Teratogen update: Lyme disease. Teratology. 2001 Nov;64(5):276-81. doi: 10.1002/tera.1074. PMID: 11745834.
- Christen H, Hanefeld F. Lyme Borreliosis in Childhood and Pregnancy. Chap. 17. In: Aspects of Lyme borreliosis. Weber K, Burgdorfer W, Schierz G (editors). Springer-Verlag; 1993.
- Theiler RN, Rasmussen SA, Treadwell TA, Jamieson DJ. Emerging and zoonotic infections in women. Infect Dis Clin North Am. 2008 Dec;22(4):755-772. doi: 10.1016/j.idc.2008.05.007. PMID: 18954762; PMCID: PMC2650502.
- O’Kelly B, Lambert JS. Vector-borne diseases in pregnancy. Therapeutic Advances in Infectious Disease. January 2020.
- Qasba N, Shamshirsaz AA, Feder HM, Campbell WA, Egan JF, Shamshirsaz AA. A case report of human granulocytic anaplasmosis (ehrlichiosis) in pregnancy and a literature review of tick-borne diseases in the United States during pregnancy. Obstet Gynecol Surv. 2011 Dec;66(12):788-96.
- McGowan KL, Hodinka RL. Laboratory diagnosis of fetal infections. Clin Lab Med. 1992 Sep;12(3):523-52. PMID: 1521426.
- Bale, James F.; Murph, Jody R. (1992). Congenital Infections and the Nervous System. Pediatric Clinics of North America, 39(4), 669–690.
- Trock DH, Craft JE, Rahn DW. Clinical manifestations of Lyme disease in the United States. Conn Med. 1989 Jun;53(6):327-30. PMID: 2667885.
- Silwa, L. Teratogenic effects of the bacteria Borrelia sp. on the fetuses of pregnant women with Lyme disease. Nowa Medycyna 4, 2011.
- Souza, IE., Bale JF., (1995). Topical Review: The Diagnosis of Congenital Infections: Contemporary Strategies. Journal of Child Neurology, 10(4), 271-282.
- Eichenfield AH, Athreya BH. Lyme disease: of ticks and titers. J Pediatr. 1989 Feb;114(2):328-33. doi: 10.1016/s0022-3476(89)80808-x. PMID: 2644410.
- Belani K, Regelmann WE. Lyme Disease in Children. Rheum Dis Clin North Am. 1989;15(4):679-689.
- Kullberg B J, Vrijmoeth H D, van de Schoor F, Hovius J W. Lyme borreliosis: diagnosis and. management BMJ 2020; 369 :m1041 doi:10.1136/bmj.m104
- Luft, B. J.; Gorevic, P. D.; Halperin, J. J.; Volkman, D. J.; Dattwyler, R. J. (1989). A Perspective on the Treatment of Lyme Borreliosis. Clinical Infectious Diseases, 11(Supplement 6), S1518–S15.
- Sood SK. Lyme disease. The Pediatric Infectious Disease Journal. 18(10), October 1999, pp 913-925
- Luft BJ, Dattwyler RJ. Lyme borreliosis. Curr Clin Top Infect Dis. 1989;10:56-81. PMID: 2679700.
- Wormser, GP. Treatment of Borrelia burgdorferi infection. Laboratory Medicine. Vol 21 (5), May 1990.
- Sicuranza, G., Baker DA. Lyme Disease in Pregnancy. Chapter 23. In: Coyle PK. (ed) Lyme disease. Mosby Year Book, 1993. p. 49-58.
- Kaslow RA. Current Perspective on Lyme Borreliosis. Grand Rounds at the Clinical Center of the National Institutes of Health. JAMA, March 11, 1992, Vol 267, No. 10
- Neubert, U. Clinical Aspects of Infections with Borrelia burgdorferi. Zeitschrift fur Hautkrankheiten 64 (8) 649-656. Eingegangen am 13.10.1988.
- Rahn DW. Lyme disease: clinical manifestations, diagnosis, and treatment. Semin Arthritis Rheum. 1991 Feb;20(4):201-18.
- Burrascano, JJ. Advanced Topics in Lyme Disease. Diagnostic hints and treatment guidelines for Lyme and other tickborne illnesses. Sixteenth edition, Copyright, October, 2008.
- Eppes, SC. Diagnosis, Treatment and Prevention of Lyme Disease in Children. Pediat Drugs, 2003:5(6):363-372.
- Conforti, C., Vezzoni R., Retrosi, C., Longone, M., Corneli, P., Magaton Rizzi, G., Nan., K., Di Meo, N., & Zalaudek I. (2020). Overview on the treatment of Lyme disease in pregnancy. Giornale italiano di dermotologia e venereologia: organo ufficiale, Societa italiana di dermatologia e sifilografia, 155(2), 220-222.
- Gould AP, Winders HR, Stover KR, Bookstaver PB, Griffin B, Bland CM, Eiland LS, Murray M. Less common bacterial, fungal and viral infections: review of management in the pregnant patient. Drugs context. 2021;10:2021-4-3.
- March of Dimes. Lyme disease and Pregnancy. retrieved online July 8, 2020: www.marchofdimes.org/complications/lyme-disease-and-pregnancy.aspx
- Schmidt BL, Aberer E, Stockenhuber C, Klade H, Breier F, Luger A. Detection of Borrelia burgdorferi DNA by polymerase chain reaction in the urine and breast milk of patients with Lyme borreliosis. Diagn Microbiol Infect Dis. 1995 Mar;21(3):121-8.
- Lawrence, RM. Transmission of Infectious Diseases Through Breast Milk and Breastfeeding. Breastfeeding (2011): 406–473. doi:10.1016/B978-1-4377-0788-5.10013-6
- Mylonas, I. (2011). Borreliosis During Pregnancy: A Risk for the Unborn Child? Vector-Borne and Zoonotic Diseases, 11(7), 891–898. doi:10.1089/vbz.2010.0102 https://pubmed.ncbi.nlm.nih.gov/20925520/
- O’Brien JM, Hamidi OP (2017) Borreliosis Infection during Pregnancy. Ann Clin Cytol Pathol 3(8): 1085
- Strobino B, Williams C, Abid S, et al. Lyme disease and pregnancy outcome: A prospective study of two thousand prenatal patients. Am J Obstet Gynecol, August 1993. https://pubmed.ncbi.nlm.nih.gov/8362948
- Williams CL, Strobino B, Weinstein A, et al. Maternal Lyme disease and congenital malformations: a cord blood serosurvey in endemic and control areas. Paediatric and Perinatal Epidemiology 1995, 9, 320-330. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-3016.1995.tb00148.
- Strobino, B., Abid, S., & Gewitz, M. (1999). Maternal Lyme disease and congenital heart disease: A case-control study in an endemic area. American Journal of Obstetrics and Gynecology, 180(3), 711–716. doi:10.1016/s0002-9378(99)70277-2 https://pubmed.ncbi.nlm.nih.gov/10076152
- Elsukova L, Korenberg E, Kozin G. The Pathology of Pregnancy and the Fetus in Lyme disease. Meditsinskaia parazitologiia i parazitarnye bolezni, Oct, 1994
- Bracero LA, Wormser GP., et al. Prevalence of Seropositivity to the Lyme disease Spirochete during Pregnancy in an Epidemic area: A preliminary report. Journal of Maternal-Fetal Investigation (1992) 2:265-268.
- Jasik KP, Okła H, Słodki J, Rozwadowska B, Słodki A, Rupik W. Congenital Tick Borne Diseases: Is This An Alternative Route of Transmission of Tick-Borne Pathogens In Mammals? Vector Borne Zoonotic Dis. 2015 Nov;15(11):637-44.
- Berger, BW. Treating erythema chronicum migrans of Lyme disease. Journal of the American Academy of Dermatology. Vol 15(3), Sept 1986.
- Mikkleson AL, Palle C. Lyme Disease During Pregnancy. Acta Obstet Gynecol Scand 66:477-478, 1987.
- Stiernstedt, G. Lyme Borreliosis during pregnancy. Scand J Infect Dis. Suppl. 71:99-100, 1990.
- Luger, SW. Active Lyme Borreliosis in Pregnancy – outcomes of six cases with stage 1, stage 2 and stage 3 disease. Abstract Book A. 4th International Conference on Lyme disease. Stockholm, Sweden, 1990.
- Schutzer SE, Janniger CK, Schwartz RA. Lyme Disease During Pregnancy. CUTIS, Vol 47, April 1991.
- Remy JM, Chevrant-Breton O, Logeais B, Patoux-Pibouin M, Chevrier S, Chevrant-Breton J (1994) Traitement de la maladie de lyme pendant la grossesse, a propos d'un cas Nouvelles Dermatologiques 13: 682.
- Buitrago, M., Ljdo, P., Simon, H., Copel J, et al. Human Granulocytic Ehrliciosis During Pregnancy Treated Successfully with Rifampin. CID 1998;27 (July). P. 213.
- Schaumann, R, Fingerle V, Buchholz K, Spencker F, Rodloff AC. Facial Palsy Caused by Borrelia Infection in a Twin Pregnancy in an area of non-endemicity. Clinical Infectious Diseases 1999;29(October).
- Tsai HC, Lu CF, Shih CM, Chao LL, Hu CH. Lyme disease during pregnancy, A case report. Dermatol Sinica 20 :147-151, 2002.
- Walsh CA, Mayer EW, Baxi LV (2007) Lyme disease in pregnancy: case report and review of the literature. Obstetrical & Gynecological Survey 62: 41–50.
- Moniuszko A, Czupryna P, Pancewicz S, Kondrusik M, Penza P, Zajkowska J. Borrelial lymphocytoma – A case report of a pregnant woman. Ticks and Tick-borne Diseases 3 (2012) 257-258.
- Hu, LT, Tsibris AM, Branda JA. Case 24-2015: A 28-Year-Old Pregnant Woman with Fever, Chills, Headache and Fatigue. Case records of the Massachusetts General Hospital. N Engl J Med 373;5, July 30, 2015.
- O’Brien JM, Baum JD. Case Report. The Journal of Family Practice Vol 66, No 8, August 2017'
- Horowitz HW, Behar C, Greene J. COVID-19 and the Consequences of Anchoring Bias. Emerg Infect Dis. 2021;27(8):2235-2236. https://doi.org/10.3201/eid2708.211107
- Markowitz LE, Steere AC, Benach JL, Slade JD, Broome CV. Lyme disease during pregnancy. JAMA. 1986 Jun 27;255(24):3394-6.
- Gerber M, Zalneraitis E. Childhood neurologic disorders and Lyme disease during pregnancy. Pediatric Neurology Vol 11(1), 1994.
- Lambert JS. An Overview of Tickborne Infections in Pregnancy and Outcomes in the Newborn: The Need for Prospective Studies. Front Med (Lausanne). 2020 Mar 6;7:72. doi: 10.3389/fmed.2020.00072. PMID: 32211414; PMCID: PMC7069275.
- Leavey K, MacKenzie RK, Faber S, Lloyd VK, Mao C, Wills MKB, Boucoiran I, Cates EC, Omar A, Marquez O and Darling EK (2022) Lyme borreliosis in pregnancy and associations with parent and offspring health outcomes: An international cross-sectional survey. Front. Med. 9:1022766. doi: 10.3389/fmed.2022.1022766